Search
- Page Path
- HOME > Search
Case Report
- A Case of Metastatic Melanoma in the Liver Mimicking Hepatocellular Carcinoma
- Jae-Kyoung So, Ji-Yun Hong, Min-Woo Chung, Sung-Bum Cho
- J Liver Cancer. 2021;21(1):92-96. Published online March 31, 2021
- DOI: https://doi.org/10.17998/jlc.21.1.92

- 6,937 Views
- 267 Downloads
- 1 Citation
-
 Abstract
Abstract
 PDF
PDF - The liver is one of the most common sites of metastasis. Although most metastatic liver cancers are hypovascular, some hypervascular metastases, such as those from melanoma, need to be differentiated from hepatocellular carcinoma (HCC) because they may show similar radiologic findings due to their hypervascularity. We encountered a case of multinodular liver masses with hyperenhancement during the arterial phase and washout during the portal venous and delayed phases, which were consistent with imaging hallmarks of HCC. The patient had a history of malignant melanoma and had undergone curative resection 11 years earlier. We performed a liver biopsy for pathologic confirmation, which revealed a metastatic melanoma of the liver. Metastatic liver cancer should be considered if a patient without chronic liver disease has a history of other primary malignancies, and caution should be exercised with hypervascular cancers that may mimic HCC.
-
Citations
Citations to this article as recorded by- A case of metastatic melanoma in the liver mimicking colorectal cancer with synchronous liver metastasis
E.A. Warshowsky, M. McCarthy, K. Wells, A. Arcidiacono, L. Csury, J.R. Nitzkorski
International Journal of Surgery Case Reports.2024; 119: 109686. CrossRef
- A case of metastatic melanoma in the liver mimicking colorectal cancer with synchronous liver metastasis

Original Article
- High-dose versus Low-dose 5-Fluorouracil and Cisplatin Based Hepatic Arterial Infusion Chemotherapy for Advanced Hepatocellular Carcinoma
- Chae-June Lim, Ji-Yun Hong, Yang-Seok Ko, Min-Woo Chung, Chung-Hwan Jun, Sung-Kyu Choi, Sung-Bum Cho
- J Liver Cancer. 2019;19(1):38-45. Published online March 31, 2019
- DOI: https://doi.org/10.17998/jlc.19.1.38
- 4,425 Views
- 170 Downloads
- 2 Citations
-
 Abstract
Abstract
 PDF
PDF - Backgrounds/Aims
Hepatic arterial infusion chemotherapy (HAIC) has been reported as an effective treatment for advanced hepatocellular carcinoma. The aim of this study is to compare the effect and safety between a high-dose regimen (750 mg/m2 5-fluorouracil [FU] and 25 mg/m2 cisplatin on day 1-4) and a low-dose regimen (500 mg/m2 5-FU on day 1-3 with 60 mg/m2 cisplatin on day 2).
Methods
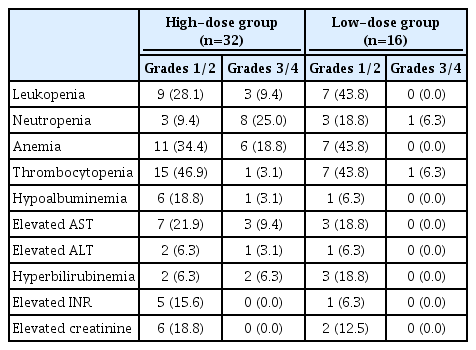
A total of 48 patients undergoing HAIC were retrospectively analyzed. Thirty-two patients were treated with the high-dose and 16 patients with the low-dose regimen.
Results
Complete response (CR), partial response (PR), stable disease (SD), and progressive disease were noted in one (3.1%), 15 (46.9%), three (9.4%), and 13 patients (40.6%) in the highdose group, and 0 (0%), one (6.3%), eight (50%), and seven patients (43.8%) in the low-dose group (p=0.002). The disease control rate (CR, PR, and SD) did not differ between groups (59.4% vs. 56.3%, p=1.000), but the objective response rate (CR and PR) was significantly higher in the high-dose group (50.0% vs. 6.3%, p=0.003). The median progression free survival did not differ between groups (4.0 vs. 6.0, p=0.734), but overall survival was significantly longer in the high-dose group (not reached vs. 16.0, p=0.028). Fourteen (43.8%) patients in the highdose group and two patients (12.5%) in the low-dose group experienced grade 3-4 toxicities (p=0.050).
Conclusions
High dose HAIC may achieve better tumor response and may improve overall survival compared to a low-dose regimen. However, the high-dose regimen should be administered cautiously because of the higher incidence of adverse events. -
Citations
Citations to this article as recorded by- A programmed cell death-related gene signature to predict prognosis and therapeutic responses in liver hepatocellular carcinoma
Xinyu Gu, Jie Pan, Yanle Li, Liushun Feng
Discover Oncology.2024;[Epub] CrossRef - Development of a novel chromatographic method for concurrent determination of 5-fluorouracil and cisplatin: Validation, greenness evaluation, and application on drug-eluting film
Souha H. Youssef, Franklin Afinjuomo, Yunmei Song, Sanjay Garg
Microchemical Journal.2021; 168: 106510. CrossRef
- A programmed cell death-related gene signature to predict prognosis and therapeutic responses in liver hepatocellular carcinoma

Case Reports
- Complete Response of Single Nodular Large Hepatocellular Carcinoma with Pulmonary Metastasis by Sequential Transarterial Chemoembolization and Sorafenib: A Case Report
- Gi-Hyun Kim, Hyung-Min Yu, Chae-June Lim, Sung-Bum Cho
- J Liver Cancer. 2016;16(1):47-51. Published online March 31, 2016
- DOI: https://doi.org/10.17998/jlc.16.1.47
- 865 Views
- 4 Downloads
-
 Abstract
Abstract
 PDF
PDF - Current guidelines recommend sorafenib as the first-line molecular target agent for advanced hepatocellular carcinoma (HCC) with extrahepatic metastasis and unresectable HCC. Sorafenib was reported to show survival benefit for patients with advanced HCC. However, complete response is extremely rare in patients treated with sorafenib. Here, we report a 52-year-old man with advanced HCC and pulmonary metastasis who showed complete response by sequential transarterial chemoembolization and continuous sorafenib. Complete response was sustained for 53-month until now.

- Long Term Survival in Patient with Hepatocellular Carcinoma after Surgical Resection of Brain Metastasis: A Case Report
- Jeong-Ho Lee, Hyung-Min Yu, Sung-Bum Cho
- J Liver Cancer. 2016;16(1):38-41. Published online March 31, 2016
- DOI: https://doi.org/10.17998/jlc.16.1.38
- 1,004 Views
- 35 Downloads
-
 Abstract
Abstract
 PDF
PDF - Brain metastasis is a rare condition of extraheptaic metastases in hepatocellular carcinoma (HCC). Patients with hepatocellular carcinoma and brain metastasis have rapidly worsened neurologic signs and symptoms, therefore it is regarded to oncologic emergency. Current recommended treatments for brain metastasis are surgical resection or gamma-knife surgery with/without whole brain radiation therapy (RT). However, patients with brain metastasis have a very poor prognosis after adequate treatment. Here, we report a 62-year-old man with HCC and brain metastasis who had long term survival after surgical resection and whole brain RT. (J Liver Cancer 2016;16:38-41)


 E-submission
E-submission THE KOREAN LIVER CANCER ASSOCIATION
THE KOREAN LIVER CANCER ASSOCIATION

 First
First Prev
Prev



 Follow JLC on Twitter
Follow JLC on Twitter